Helping Human Resources Managers Prepare for Coronavirus Pandemic
March 10, 2020 – Legal AlertsThis article covers the many laws a Human Resources manager needs to consider while implementing practical business solutions required during a pandemic, as well as provides a summary of the recommendations of the Centers for Disease Control and Prevention (CDC) and other agencies, with some tips and resources for a comprehensive guide.

Background
The last pandemic in the U.S. was in 2009, when the H1N1 flu swept through the country. The CDC estimated there were as many as 60.8 million cases of H1N1 in the U.S. during the 2009-2010 timeframe. Of those cases, over 250,000 people were hospitalized, and approximately 12,500 deaths were attributed to H1N1. Children and young adults were at greatest risk during the 2009 H1N1 pandemic. Many may remember schools, day care centers, summer camps, and universities closed down to stop the spread of the H1N1 flu. During that time, the federal government’s many agencies developed pandemic plans and policies, as did businesses. With what is happening now in the U.S., the time has come for businesses to update those policies for what appears to be a possible COVID-19 pandemic.
The COVID-19 virus is highly infectious, but its symptoms tend to be mild in most (80 percent) of people. It does not present as a runny nose or nasal congestion. Rather, 90 percent of patients have a fever and 70 percent have a dry cough. Those who are acutely ill usually experience shortness of breath. For people with cardiovascular disease, diabetes, high blood pressure, or compromised immune systems, COVID-19 is causing severe illness and, for some, death. As a result, this possible pandemic is impacting the elderly and anyone already suffering from chronic illness more than children. In fact, the World Health Organization (WHO) reported that few children contracted the disease in China and none of those died. For comprehensive information on the Coronavirus go to: www.cdc.gov.
Summary of CDC Recommendations for Employers
Remember, as you review the CDC recommendations, it does not relieve employers of obligations they may have under the Americans With Disabilities Act (ADA), the Family Medical Leave Act (FMLA), the Fair Labor Standards Act (FLSA), the National Labor Relations Act (NLRA), or other applicable federal or state laws, some of which are discussed below in the context of pandemic planning. It is also important to remember public health orders can trump all other relevant laws, especially when they impose a quarantine.
(See: www.cdc.gov/quarantine/aboutlawsregulationsquarantineisolation.html)
1. Actively encourage employees with respiratory illness and fever to stay home until they are free of a fever for at least 24 hours. You may still require they notify their supervisor daily.
2. Ensure your sick leave policies are modified to be flexible enough they are consistent with any public health guidance, and employees are aware of these modified policies.
3. Talk with companies that provide your business with contract or temporary employees about the importance of their sick employees staying home, and encourage them to develop non-punitive leave policies consistent with CDC guidelines.
4. Consider whether you really need to require a health care provider’s note for employees who are sick with acute respiratory illness to validate their illness, as health care provider offices and medical facilities may be extremely busy and not able to provide such documentation in a timely way. (One useful approach during a pandemic may be to only require notes of those who have a record of excessive absences.)
5. Employers should have flexible policies permitting employees to stay home to care for a sick family member. Employers should be aware more employees may need to stay at home to care for sick children or other sick family members than usual.
6. Be prepared to separate sick employees. The CDC recommends employees who appear to have acute respiratory illness symptoms (i.e., cough and shortness of breath) upon arrival to work, or become sick during the day, should be separated from other employees and sent home immediately. Sick employees should be told to cover their noses and mouths with a tissue (or an elbow or shoulder if no tissue is available) when coughing or sneezing.
7. Place posters in the workplace that: a) encourage staying at home when sick; b) explain the proper etiquette for coughing and sneezing; c) explain hand hygiene when entering the work place or other working areas; c) explain how to wash hands; d) explain how to use anti-bacterial gels; and e) explain employees should use soap and water if their hands are visibly dirty.
8. Provide tissues and no-touch disposal receptacles for use by employees. Provide alcohol-based hand sanitizer with 60-95 percent alcohol. Ensure supplies are maintained in multiple locations or in conference rooms.
9. Perform routine environmental cleaning of all frequently touched surfaces (e.g., workstations, countertops, doorknobs, etc.). No additional disinfection beyond routine cleaning is recommended at this time.
10. Provide disposable wipes so commonly used surfaces (e.g., doorknobs, keyboards, remote controls, desks, etc.) can be wiped down by employees before each use.
11. For employees who are traveling, check the CDC Travelers’ Health Notices for guidance on each country of travel. Specific travel information for travelers going to and returning from China and information for aircrew can be found on the CDC website. Advise employees to check themselves for symptoms of acute respiratory illness before starting travel, notify their supervisor, and stay home if they are sick.
12. Ensure employees who become sick while traveling or on temporary assignment understand they should notify their supervisor and promptly call a health care provider for advice if needed.
13. Employees who are well but have a sick family member at home with COVID-19 should notify their supervisor and refer to CDC guidance for how to conduct a risk assessment of their potential exposure.
14. If an employee is confirmed to have COVID-19, employers should inform fellow employees of their possible exposure to COVID-19 and maintain confidentiality as required by the ADA and Health Insurance Portability and Accountability Act (HIPAA). Employees exposed to a co-worker with confirmed COVID-19 should refer to CDC guidance for how to conduct a risk assessment of their potential exposure.
15. Consider how best to decrease the spread of acute respiratory illness and lower the impact of COVID-19 in their workplace in the event of a more severe outbreak in the U.S. Identify and communicate objectives, which may include one or more of the following:
- reducing transmission among staff (e.g., via social distancing or working from home);
- protecting people who are at higher risk for adverse health complications (i.e., permitting offering accommodations for higher risk individuals until pandemic situation has passed);
- maintaining minimum business operations; and
- minimizing adverse effects on other entities in supply chains.
16. Some key considerations when making decisions on appropriate responses include the following:
(a) disease severity in the community where the business is located;
(b) impact of disease on employees who are vulnerable and at higher risk for adverse health complications;
(c) prepare for possible increased numbers of employee absences due to illness of employees and their family members or dismissals or closures of schools;(d) monitor and respond to absenteeism at the workplace. Implement plans to continue your essential business functions in case you experience higher than usual absenteeism;
e) cross-train personnel to perform essential functions so the workplace is able to operate even if key staff members are absent;
f) assess essential functions and reliance others place on your services or products. Be prepared to change your business practices, if needed, to maintain critical operations (e.g., alternative suppliers, prioritize customers, or temporarily suspend some of your operations if needed);
g) if you have more than one business location, provide local managers with authority to take appropriate actions based on the conditions in their locality; and
h) coordinate with state and local health officials.
Other Possible Suggestions Not Yet Recommended by the CDC
1. If your employees travel by car, consider outfitting them with supplies to protect them while stopping to refuel.
2. Encourage employees to practice the six foot rule when in public spaces and they notice someone with symptoms, encourage them to keep a six-foot distance to lessen their risk.
3. During the 2009 H1N1 pandemic, as more and more people became infected, the CDC suggested screening employees when they arrived at work. Currently, the CDC recommends this for employers in health care, death care, waste management, solid waste, airline travel, border patrol, and international travel businesses.
4. Another recommendation of the CDC in 2009 was one that is available under the ADA, which is making appropriate plans for changing the work duties, work spaces, or schedules for employees at higher risk for complications from COVID-19.
5. As your business explores ways to increase social distancing at work, consider the following tools: a) cancel non-essential face-to-face meetings; b) cancel non-essential business travel; c) use conference calling; and d) offer telework or flexible hour options.
The Family Medical Leave Act (FMLA)
FMLA covers employers with 50 employees or more within a 75 mile radius. To be eligible for FMLA leave, an employee must have worked for the employer for 12 months (and at least 1,250 hours). Under FMLA, employers must provide employees with up to 12 weeks unpaid leave to care for a spouse, son/daughter, or parent with a serious health condition or for the employee’s own serious health condition. Employers should anticipate that health care providers will likely view being quarantined as a result of COVID-19, or caring for someone seriously ill from the virus, as meeting the definition of a serious health condition.
Even if COVID-19 is at issue, the employer can still require employees to give the employer notice as soon as practical, require the absent employee comply with the employer’s daily call-in procedures, provide information to support that absence is due to a serious health condition, and estimate the probable length of absence. If your locality is particularly hard hit, employers may need to consider relaxing some of the FMLA deadlines for the return of various medical information if providers are simply overwhelmed.
Employers need to inform employees if leave will be FMLA protected and the amount of leave to be counted against their FMLA leave time. If the employer determines a requested leave will not be covered by FMLA, they’ll need to inform the employee of that as well. At option of either the employee or the employer, FMLA allows substituting any accrued paid leave for unpaid leave. In fact, the employer can require an employee use accrued paid leave while also counting the absence as FMLA leave.
Americans with Disabilities Act (ADA)
The ADA generally applies if the employer has 15 or more employees. The ADA protects a disabled person from discrimination in the workplace when he/she is qualified to perform the essential functions of the job, with or without a reasonable accommodation. A disability is any physical or mental impairment that substantially limits one or more of an individual’s life activities. Reasonable accommodations can include: rearranging existing facilities or workplaces; job restructuring; part time, modified or flex time schedules; adjustment of policies; reassignment to a vacant position; and/or a leave of absence. However, an accommodation is not reasonable if it imposes an undue hardship on the employer.
Determining what is reasonable requires an informal interactive process. An employer need not agree to a particular accommodation requested if it is unreasonable. Furthermore, if an employee refuses a reasonable accommodation and cannot perform the essential functions of the job, he/she is no longer a qualified person under ADA.
Persons with chronic health conditions (e.g., diabetes, cancer, coronary heart disease, immune deficiency disorders, etc.) may, depending on individual circumstances, qualify as disabled or be perceived to be disabled, and there is little dispute they are at higher risk of complications with COVID-19. Thus, the ADA will likely play an important role for employers during this potential pandemic.
This begs the question: If you are aware of an employee’s chronic health condition, may you lawfully inform others of an employee’s health condition and their possible need for an accommodation? Once a person is hired, an employer may inform supervisors and managers of necessary restrictions or accommodations. The law also allows an employer to inform first aid and safety personnel when appropriate. However, the ADA says nothing about allowing the sharing of information with co-workers. Thus, if the employee seeks an accommodation, you would be able to discuss the issue with the employee and his/her manager or supervisor to work out an accommodation that reduces risk.
What about taking the initiative, with the best of intentions, to ferret out persons with chronic illnesses ahead of time, so you can help them? While the ADA allows pre-employment inquiries into the ability of an applicant to perform job related functions, it does not allow an employer to require responses to medical inquiries for current employees, unless it is job related and consistent with business necessity. There is some good news though, the ADA does allow for some planning in situations like this. An employer can conduct voluntary medical histories, subject to confidentiality requirements. Specifically, an employer can survey its workforce for personal information needed for pandemic preparation, but only if the employer asks broad questions, not limited to disability-related inquiries.
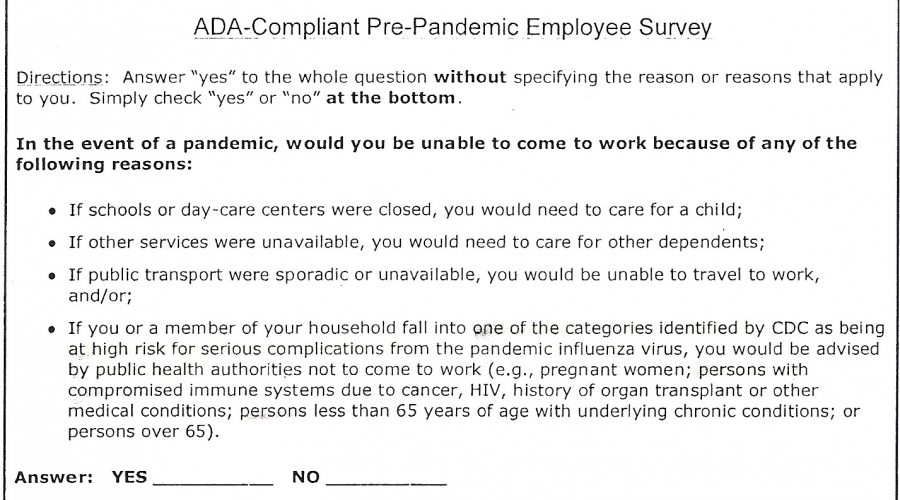
Attachment A is an example of a sample ADA compliant survey acceptable in 2009. Such a compliant survey could be prepared by a business for a possible COVID-19 pandemic. You can also consider whether it would be helpful to announce in advance that absences for up to seven days will be excused for all persons who self-disclose in the survey.
Finally, nothing in the ADA prohibits the employer from adopting non-invasive infection control practices at work, such as: 1) requiring regular hand washing, as well as coughing and sneezing etiquette; 2) tissue usage and disposal etiquette; 3) personal protective equipment (e.g., face mask, gloves, gown, etc.), although the employer may need to accommodate for allergies due to latex and provide modified gowns for use with wheelchairs; and 3) encourage or require telework.
Separated workspace and telework may also be considered reasonable accommodations for persons needing an accommodation during the pandemic. Also note, employers must not discriminate against any protected class in requiring, granting or denying telework options.
Fair Labor Standards Act (FLSA)
The FLSA regulates hours and wages of employees engaged in interstate commerce. It sets statutory minimum wages for all hours worked and requires overtime pay for hours over 40 in a work week. Employing someone means “to suffer or permit to work,” which becomes important in these situations. Employees doing non-requested work, with the knowledge of an employer, must be paid, and that includes “homework” performed with employer’s knowledge, unless it is work done by an exempt employee.
Under FLSA, it is the employer’s duty to stop an employee from doing work the employer does not want done. FLSA also requires these policies to be “published” to employees with specific instructions on how long to work. FLSA does not require paid sick leave. As such, paid absences do not count as work time under FLSA. However, on-duty time spent waiting for work counts as work time, and “comp time in lieu of overtime” must be limited to the same pay period, which obviously restricts the future use of comp time. All of this requires very careful recordkeeping. Employees are not allowed to waive their right to overtime or minimum wage, even in emergency or crisis situations. Finally, employees cannot volunteer their work time to an employer.
If an employer is going to permit non-exempt employees to work from home, there must be clear instructions, in writing, about the number of hours being worked, including wait times. For all employees paid by the hour, since they will be working in their residence, there should be clear guidelines about whether meal time and breaks will be paid while the employee is working from home. Careful records of time should be kept and reviewed regularly.
Meanwhile, back at the office or plant, keep track of overtime hours for persons having to stay longer hours due to substantial absences of others. Monitor exempt employees working longer hours so they do not fall below minimum wage. Remember exempt employees who take over the manual job duties of non-exempt employees may become subject to overtime provisions. (Even if the exempt employee does not complain or seek it, a union official or disgruntled employee can report the situation to the USDOL.) Finally, FLSA does not limit the types of work employees may be assigned or required to perform, except for persons age 17 or younger.
Workers’ Compensation Issues
State workers’ compensation laws are designed to offer medical and financial benefits to workers "injured" in the scope of their employment. This includes physical injuries resulting from accidents on the job (many states have eliminated the "accidental" requirement), as well as occupational diseases due to causes and conditions characteristic of, and peculiar to, a particular occupation. Employees claiming on the job exposure to communicable diseases, testing either positive or negative, have been awarded benefits. The typical employee is usually a health care worker, prison guard, or housekeeper in a facility housing persons who have communicable diseases.
For an accidental injury, an employee must prove when and where the transmission occurred (i.e., on the job). For an occupational disease, the employee must prove a substantial connection between the worker’s occupation and the transmission of the disease. Employers will need to check how their state handles occupational disease claims of HIV/AIDS, tuberculosis, and other communicable diseases to better understand what may happen with COVID-19. Because COVID-19 may become widespread, determining specifically when and where it was contracted may be difficult. Expect compensable claims will be limited to those who have a substantial connection between their occupation and the transmission of the disease (e.g., health care workers, possibly overseas flight attendants, etc.).
National Labor Relations Act (NLRA) & Unionized Employers
There will be issues unique to unionized employers, from negotiated attendance control policies, contracting out bargaining unit work, supervisors performing bargaining unit work, prohibition on assignments outside job classification, contractual restrictions on overtime, and restrictions on needed flexibility.
If the employer is not in a position to obtain cooperation from the union at the time, it should look at what emergency provisions are in its collective bargaining agreement and any past arbitration decisions interpreting emergency situations under its past contracts. Consider negotiating a memorandum of understanding (MOU) with the union to cover possible pandemic needs to maintain the business. If that does not work, anticipate allegations of unilateral changes and the defense of exigent circumstances. When claiming exigent circumstances, the burden of proof is on the employer.
Consider whether to negotiate with the union about:
- temporary modification of absenteeism policies and procedures and
- temporary changes to workplace rules and contracting out in order to maintain business during a pandemic situation.
Each employer’s circumstances with its union is different; one size does not fit all. However, expect most arbitrators will be unlikely to uphold discharges for excessive absenteeism when there is proof of pandemic illness in a particular workforce or community, despite an employee’s past history.
Occupational Health & Safety Act (OSHA)
OSHA requires employers provide safe and healthful working conditions. With this mandate in mind, OSHA has the authority to create standards employers must follow and can issue advisory guidance, including for standards applicable to COVID-19 in the workplace. See https://www.osha.gov/SLTC/covid-19/standards.html.
For employers whose employees are not at a high risk of exposure, OSHA has simply referred employers to the CDC guidelines summarized above. However, for employers involved in businesses deemed higher risk (e.g., health care, death care, labs, airlines, international travel, border protection, solid waste, wastewater management operations, etc.) or are working in a business with someone already diagnosed with COVID-19, there is other guidance. These businesses should visit OSHA’s hazard recognition webpage for instructions on evaluating the risk of exposure; implementing and ensuring workers use controls to prevent exposure; and taking various control measures that may include engineering and administrative controls, safe work practices and using personal protective equipment (PPE).
HIPAA Privacy Considerations for Employers during the COVID-19 Outbreak
At times like this, employers may wish to know if an employee who has left work with a fever or cough and is not coming to work is out due to a suspected or diagnosed case of COVID-19 and whether they may notify co-workers who have been in close contact with that employee. To what extent does HIPAA cover this type of information?
The HIPAA Privacy Rule applies to disclosures made by employees, volunteers and other members of a covered entity’s or business associate’s workforce. “Covered entities” are health plans, health care clearinghouses and those health care providers that conduct one or more covered health care transactions electronically, such as transmitting health care claims to a health plan. “Business associates” generally are persons or entities (other than members of the workforce of a covered entity) who perform functions or activities on behalf of, or provide certain services to, a covered entity that involve creating, receiving, maintaining, or transmitting protected health information or (PHI). Employer health plans are covered by the HIPAA Privacy Rule, but employers generally are not otherwise covered (unless their line of business qualifies them as either a covered entity or business associate). However, the HIPAA Privacy Rule permits covered entities to disclose needed PHI without the individual authorization, when the disclosure is made to further the following public health activities:
- disclosures made to a public health authority, such as the CDC or a state or local health department authorized by law to collect or receive such information for the purpose of preventing or controlling disease, injury, or disability;
- disclosures at the direction of a public health authority to a foreign government agency acting in collaboration with the public health authority; and
- disclosures to notify a person who may have been exposed to a communicable disease or may otherwise be at risk of contracting or spreading a disease or condition, if disclosure is authorized by law or otherwise permitted using minimum necessary standard.
The Office of Civil Rights (OCR) at the U.S. Department of Health and Human Services (HHS), the agency responsible for oversight of HIPAA regulations and enforcement, has issued a bulletin regarding the ways covered entities can share patient information under the HIPAA Privacy Rule in an outbreak of infectious disease or other emergency situation. The OCR bulletin is available here.
In short, the HIPAA Privacy Rule will have limited applicability in a COVID-19 response planning of employers, but privacy concerns of employees are still important. The key is to ensure the employer’s COVID-19 plans do not involve or rely on PHI obtained from the employer’s health plan. For example, if an employee with COVID-19 submits a request for leave along with the results of his/her virus screening, the HIPAA Privacy Rule would NOT come into play. Why? Because the information was voluntarily provided to the employer by the employee for employment purposes entirely unrelated to the employer’s health plan activities. This information was provided to the employer and not to the health plan. Once in the possession of the employer, the HIPAA Privacy Rule does not per se impose any obligation to maintain the employee’s information confidentially. However, regardless of good intentions, do not take this as a license to disclose this information to other employees. Why?
Some will say, refer to the ADA as the reason not to disclose, but the ADA prohibits an employer from sharing medical information regarding an employee’s disability with the employee’s co-workers. However, it does permit such disclosure to supervisors, managers, and emergency personnel who need to know. A diagnosis of COVID-19 would not ordinarily, by itself, be considered a disability under the ADA. That is still not a reason to make unfettered disclosures. These disclosures would still likely be considered a breach of the common law right of privacy or possibly support a defamation claim, and these are recognized in many state jurisdictions. For this reason, it is better to avoid identifying an individual to one’s co-workers. We recommend instead that the HR manager train supervisors to maintain confidentiality and provide guidance as to how to respond to employee questions. Consider whether it makes sense for the company to designate someone as the person responsible for handling all COVID-19 employee information and inquiries, such as an HR manager or safety manager. Provide appropriate advance written notice to the employee if it becomes necessary to disclose information about an employee’s COVID-19 status to protect those in the workforce who came in close contact with that employee, especially if the situation is going to require employees being placed under quarantine or self-monitoring at home. In fact, it may become essential to advise particular employees who were in close contact (employees who worked within six feet of each other for prolonged periods) they should be tested for COVID-19). Check to see if your state has any particular medical privacy rules for applicability as well and what public health orders have been issued.
Conclusion
When written in Chinese, the word “crises” is composed of two characters. One represents danger and the other represents opportunity. As your business faces the possibility of danger to its valuable human resources, this is the opportunity for HR managers to help alleviate the potential and real strain on both your people and the business. If you have questions on any aspect of employment laws related to the potential COVID-19 pandemic, contact any of Dinsmore’s labor & employment attorneys. If you have any questions regarding the impact of the HIPAA Privacy Rule on your COVID-19 outbreak planning or have general questions regarding HIPAA compliance, please contact any of our Dinsmore health care attorneys. Dinsmore’s website is: https://www.dinsmore.com
Attachment A